Community Health Centers (CHCs) fill an important role in our healthcare industry. These organizations provide care to patient populations that have previously been underserved and, as a result, suffered negative health outcomes. These are patient populations struggling with socioeconomic difficulties, food insecurity, and inadequate housing. CHCs have come along and made a difference in these individual’s lives by providing quality care, and many are now implementing remote patient monitoring programs to take that care to an even higher level. Read on to learn more about how RPM can benefit CHC patient populations and what you need to do in order to implement such a program in your community health organization.
 What is remote patient monitoring?
What is remote patient monitoring?
Remote patient monitoring (RPM) is a form of telehealth that allows providers to manage patients’ acute and chronic conditions outside of the practice walls utilizing digital medical devices that collect data and transmit it to the patient’s care team. Devices used for RPM include blood pressure monitors, wearable ECGs, pulse oximeters, scales, and blood glucose monitors. These devices aid providers in monitoring conditions such as diabetes, cardiac disease, asthma, hypertension, and more. Providers can create workflows that allow data indicating a potential problem to prompt an actionable alert to the provider.
4 Ways CHC Patient Populations Can Benefit from RPM
While RPM is beneficial to all patient populations, those served by CHCs often face challenging socioeconomic circumstances that can negatively affect their health, making RPM particularly impactful in these situations. Here are four benefits CHC patient populations can see from the use of RPM:
- Improved clinical decision-making: The data that providers gain access to through RPM enables providers to identify trends in their patients’ conditions more accurately, allowing them to notice anomalies more quickly. This aids providers in making the best possible treatment choices.
- Improved self-monitoring and treatment adherence among patients: RPM provides patients with the tools to manage their condition more adequately. Additionally, patients gain a greater sense of understanding of their condition and the importance of their treatment plan, leading to better adherence over time.
- Improved care access: RPM enables patients to be continually under their provider’s care without increasing the frequency of their visits. This also leads to better health outcomes while overcoming the barriers that may have kept patients from receiving care in the past.
- Improved patient/provider relationships: RPM not only enables providers to keep a closer eye on their patients, creating a deeper understanding of each patient’s condition, it also provides more opportunities for communication, creating a stronger connection between patient and provider. Additionally, using this tool gives patients the comforting feeling that their provider is watching over them, increasing trust.
3 Important Considerations When Implementing RPM in Your CHC
Implementing any new program requires a great deal of planning. Here are three important things to consider when planning an RPM implementation at your CHC:
- Which condition is most important to start with? Looking at your patient population, which condition do you see a particularly high rate of? By identifying the most common issue that your patients are struggling with, you cand determine the best place to start in order to have the opportunity for a meaningful impact.
- What kind of devices will work best for your patient population? CHCs typically serve patients living in difficult socioeconomic situations who may not have access to Wi-Fi, smartphones, and other similar technologies. It’s important to choose an RPM solution that overcomes the barrier of limited access to technology by utilizing devices with a cellular connection.
- How will you fund this program? Unfortunately, CHCs are not eligible to receive reimbursement for RPM services at this time. With this in mind, it’s important to consider how your budget could be adjusted, additional revenue brought in, or if a grant can be obtained to support this endeavor.
The opportunity to provide a higher level of care for a patient population that has traditionally been underserved, such as those who most often benefit from the work of CHCs, is a fantastic reason to implement remote patient monitoring in such an organization. While there may be hurdles to overcome, particularly regarding finances, the work to get past these obstacles is worthwhile when you begin to see improved patient health outcomes.
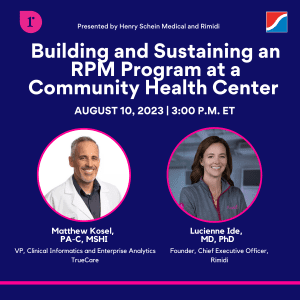
When looking for an RPM solution that is ideal to serve a CHC patient population, look no further than Rimidi, offered by Henry Schein SolutionsHub. Rimidi uses digital medical devices with a cellular connection to seamlessly collect patient data regardless of patient access to technology. That data is aggregated and notifications are sent to providers directly in their EMR system when a reading requires their attention and action.




